The silent struggle of postpartum depression
 Read To Me
Read To Me
Sign up for a six month free
trial of The Stand Magazine!
After the birth of a baby, an estimated 1 in 7 women are diagnosed with postpartum depression (PPD), according to Brown University Health.
Johns Hopkins Center for Women’s Reproductive Mental Health reports that while 85% of new mothers experience the “baby blues” within the first few weeks of childbirth, PPD is a more serious and lasting mental struggle. PPD causes extreme sadness, anxiety, and hopelessness that can interfere with a woman’s ability to care for herself or bond with her baby. Other red flags for PPD are trouble sleeping or sleeping too much, intense mood swings, withdrawal and lack of interest in people and activities previously enjoyed, and sudden weight loss or weight gain.
The greatest risks of PPD are thoughts of self-harm, harming the baby, or suicide.
While PPD usually begins in the first few months after giving birth and ends within the first year, a 2020 study by the National Library of Medicine discovered it can last for up to three years, if not addressed. PPD can also arise after miscarriage, stillbirth, or abortion, cases which receive less clinical follow-up and are therefore less likely to lead to professional diagnosis and treatment.
According to research published in January 2025 by the National Library of Medicine, “Perinatal depression stems from a combination of hormonal changes, genetic predisposition, and environmental factors, yet up to 50% of cases remain undiagnosed due to the stigma surrounding the condition and patients’ reluctance to disclose symptoms.”
Because many women don’t correctly identify the symptoms or understand where or how to seek help, they end up feeling helpless, ashamed, and alone. Therefore, it is imperative for loved ones to recognize and respond to the symptoms of PPD.
Here, two experts offer help and hope to both mothers and fathers who are facing the struggles of PPD.
For new mothers, hurting wives
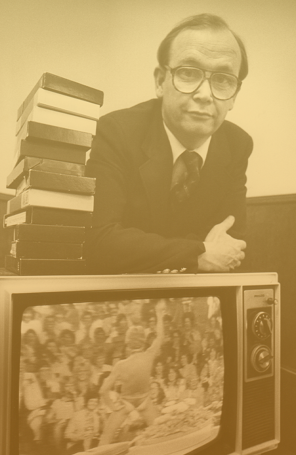
Women are typically unprepared and confused when faced with PPD. This was the experience of Jerusha Clark, pastor’s wife and author of numerous books on parenting, relationships, and mental health, including Living Beyond Postpartum Depression.
“I had no frame of reference for postpartum depression,” Clark said on an episode of Focus on the Family with Jim Daly. On the episode, titled “Embracing Hope in the Midst of Postpartum Depression”, which aired February 15, 2019, she added, “I literally had no idea that it was possible for a Christian to feel like there was no other option but to die.”
Reacting to the darkness
Clark’s depression led to her being hospitalized the day her first daughter turned four months old. Clark then attempted suicide after the birth of her second daughter.
While lack of sleep, sudden emotions, and physical changes are to be expected when adjusting to a new baby, Clark warned that women should seek clinical evaluation if they have symptoms of PPD for two to four weeks – especially more than a month – without any days of feeling joy.
As a Christian woman, Clark found it was an even greater struggle to acknowledge feelings that seemed to conflict with her faith and the commitment to be a good wife and mother.
“Did I do everything wrong? Did I mess this up? … I was having all these questions, and the shame was so heavy,” Clark said. “I was a bad mother in my mind. … I had the Holy Spirit in me, and yet I had these dark thoughts – I didn’t even have a place to put them.”
Receiving help
While Clark had a quick recovery with medication and treatment, she also found that spiritual healing strengthened her faith and deepened her relationship with God.
“God unraveled a lot [of things] in my mind and heart that I didn’t know were there, but He met me on every level,” she said. “Physically, I needed to be healed; emotionally, there were a lot of things to sort through like, Why am I so convinced that I have to be a perfect mom?”
Clark now shares her experience to help others find hope, healing, and faith (standingstoneministry.org).
“I know what it’s like to be there, and I know God can be victorious,” she said. “Part of the reason I tell my extreme story is so that [these women] can have courage that ‘If she went to that dark place, then I can face this, and God can bring me back.’”
For new fathers, supportive husbands
When a husband notices his wife is struggling after childbirth, knowing how to respond can make all the difference. Hannah Littlepage, a licensed professional counselor (LPC) in Springfield, Missouri, specializes in maternal mental health, and she emphasizes the need for concerned husbands to educate themselves about postpartum depression.
“This is a crucial first step,” she told The Stand. “A husband can support his wife by learning to recognize signs of postpartum depression,” while understanding that it is a legitimate medical, emotional, and mental condition that often needs professional intervention.
Rehearsing the conversation
“How a concerned husband broaches the subject with his wife is important,” Littlepage added. “It should be gentle, almost like he’s going into an intensive care unit, recognizing how vulnerable and fragile the patients are. He should be that gentle with his wife’s heart as he approaches her to talk about her struggles.”
Littlepage emphasized that the conversation should focus on the husband’s observations using “I” statements, such as, “I feel worried about how exhausted you seem,” rather than making accusations toward his wife. Husbands should avoid trying to “fix” their wives’ feelings or solve their problems. Instead, they should focus on listening and being present.
She also pointed out three crucial messages husbands should convey to their wives: “You’re not alone. You’re not to blame. And with help, you will be well.”
Resorting to practical steps
But what can a husband do when he doesn’t know what to do?
Littlepage explained that husbands should act rather than ask how to help.
“Decisions can feel overwhelming. To alleviate some stress, a husband can … take the initiative and say, ‘I’m going to do this,’” Littlepage advised.
This includes helping with feedings and diaper changes, running errands, scheduling appointments, and ensuring wives have opportunities to rest and maintain hygiene. Husbands should manage external pressures by setting boundaries with family and friends, returning calls, and coordinating care for other children.
It’s also important to acknowledge that supporting a wife through postpartum depression can be emotionally taxing on the husband too. That’s why Littlepage encourages husbands to recognize the situation as a time for personal spiritual growth: “This is an opportunity to learn how to understand your own emotions, take those to the Lord, and ask Him to minister to you so you can minister to your wife.”
Editor’s Note: This article is not intended to provide medical advice, nor should it be used to diagnose or treat postpartum depression. It is intended for educational and informational purposes only and should not delay or replace seeking professional help.

Sign up for a free six-month trial of
The Stand Magazine!
Sign up for free to receive notable blogs delivered to your email weekly.